Dr. Thea James has worked in healthcare for nearly 30 years. She understands that health isn't just about eating right and exercising; it's influenced by lack of access to jobs and green space, housing instability, air pollution, and more.
In the United States, your zip code is a powerful predictor of how long you live. For someone in Newton, Massachusetts, life expectancy extends well into the 90s. But drive just an hour south to New Bedford, and you’ll find it drops to an average of just 68 years old.
It’s tempting to boil down good health solely to factors like medical care, healthy food, and exercise. However, these things alone don’t explain that 25-plus year gap between these two communities. Many other dynamics contribute to the difference there and in neighborhoods throughout New England. Historic policies like redlining and racial segregation, along with substandard housing, air pollution, crumbling infrastructure, and lack of access to jobs, healthy food, and green space all play a role.
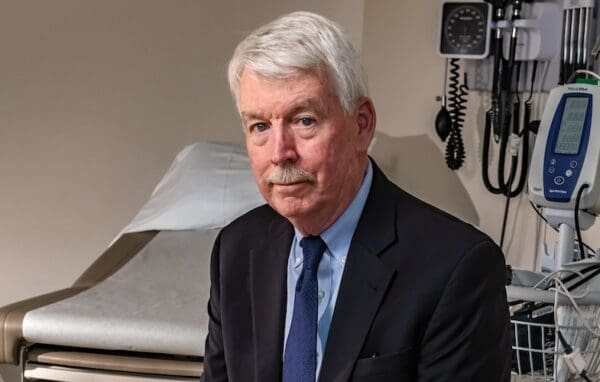
Perhaps no one understands the interplay of these factors better than those who work in healthcare. Dr. Thea James, who serves as Boston Medical Center’s Associate Chief Medical Officer, Vice President of Mission, and Director of the Violence Prevention Program, began her career at the hospital nearly 30 years ago. In her work, she sees firsthand how the places where you live, work, and play impact health – both physically and mentally. As a member of CLF’s Board of Trustees and co-chair of the CLF Ventures Board, Dr. James advises the organization on its work to create healthier neighborhoods and economic opportunities through its Healthy Neighborhoods Equity Fund. Boston Medical Center is an institutional investor in the Fund.
We recently checked in with Dr. James to understand how the Center is dealing with the COVID-19 pandemic and to hear from her about the work still to be done to create healthier, more thriving, and more equitable neighborhoods for all.
This transcript has been edited for clarity and flow.
What prompted you to choose emergency medicine as your specialty?
I never actually entertained other specialties. I liked the notion of not knowing what’s coming next. I also recognized that people show up to the emergency room with all forms of emotions: fear, angst, sadness, depression, sometimes just anger. And, as a provider, I would have the opportunity to shift that person’s perspective by just being there, hearing where they’re coming from, and sort of walking them to a better place.
Nobody listens to patients, really. Doctors listen for what they’re taught to listen for – the disease and what’s going on with the disease. You’ve got a bellyache and the doctor will ask, “Okay, when did it start? Does eating make it worse? What makes it feel better?” But your bellyache could be due to you not having enough food, or you’re in a domestic violence situation, or you have something else going on. So, that’s what drew me to emergency medicine – listening beyond the script and wanting to shift a person’s perspective.
How does where you live affect your health?
When you think about the way that communities across America have been created and segregated – long, long ago, with great intentionality, I might add – people of color have wound up in neighborhoods that are risky from an environmental perspective. They’re either close to power plants or living in places where there’s pollution in the air or there’s something in the water, like in Flint, Michigan. Even something as basic as not having a lot of tree coverage has an effect because that means there’s more heat there.
These communities don’t have the things they need to create a healthy, thriving community or even a thriving economy within a community. One of the greatest impacts of that historic segregation is economic. By not having access to wealth-building pathways like homeownership – which was denied to Black communities starting in the 1930s through redlining, at the same time the government created public housing – essentially two socioeconomic populations were created and that remains fixed to this day.
All the statistics show that people who have lower incomes and lower educational attainment – they have worse health status. The data also show that their children do, too, because the children are just beneficiaries of what resources the parents have.
When you look at COVID-19, for example, and the high rates of occurrence and death, it correlates with all those cities that were behind the red lines. When people are living in those kinds of conditions and under those circumstances, they can’t even prioritize health because they’re busy trying to survive. They will address survival first, and then health will come second, if at all.
What do we, as a society, need to do to create healthier neighborhoods?
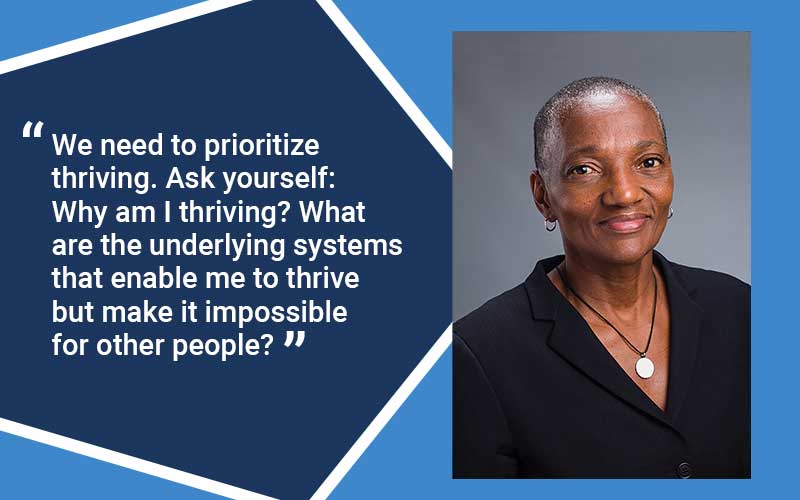
We need to prioritize thriving. Ask yourself: What does it require for a person to thrive? Why am I thriving? We need to look at this from a systemic perspective: What are the underlying systems that enable me to thrive but make it impossible for other people. People who are not thriving – that’s not natural. It’s not biologic or in their DNA. It’s not like a disease. This is man-made stuff.
Changing that is going to involve policy, because a lot of the systemic barriers and systemic racism that have occurred were driven by policies. So, we have to undo those things.
And I think history is really important. Because if you don’t understand the history of how we got here, there’s no way you could ever know how to undo all of this. That requires intentionality. The most common thing people will come up with to do is the thing they’ve always done. And that’s not enough. We don’t want to inadvertently recreate the same type of systemic barriers. To change the situation, you have to add something else onto that, and that has to be something that prevents people from getting into that situation in the first place.
How does a program like the Healthy Neighborhoods Equity Fund help?
This program lives the notion of conservation. It really walks the walk, especially when you create something like a Healthy Neighborhoods Equity Fund way before “equity” was the word of the day. And, then, you put guardrails on it by setting up a healthy impact scale to make sure it’s 100% pure through and through – those impact scale measures are rooted in equity. Even if you’re a housing developer, you have to meet these measures. That is pure and true and a model for everybody. It’s not that hard – I just feel like it’s not that hard for people to shift. The only thing that stops them from shifting is their mind.
What gives you hope?
I am hopeful because, right now, we’ve gotten a bit of a boost this year with this insight, this new awakening to systemic injustice. But it cannot be a flash in the pan. This is going to be a long haul, but it’s okay. We have to recognize that and have intentionality around it. My greatest fear, and, I’ll tell you, it’s the greatest fear of every person of color I know, is that the country will just go back to business as usual. You fear it because we can’t imagine that anybody is interested in changing the situation.
If this was all theoretical to me, I might not have the hope that I have. But I’ve seen proof of concept. I’ve seen this happen. Here at Boston Medical Center, I’ve seen these kids in our violence intervention program go from someone without hope to maybe they get their GED, then to a kid who has a college degree and, in many cases, a graduate degree after that. It just says to me that these things are changeable and it’s within our grasp.